Achieving cure for pancreatic cancer- Surgery beyond Whipple’s operation
Pancreatic cancers is one of the most aggressive type of cancer with a high mortality rate.
Surgery remains the gold standard for treatment of pancreatic cancer which has not spread. The standard procedure for pancreatic cancer is known as a Whipple’s operation in which the duodenum and part of the bile duct and pancreas is removed
There are a group of pancreatic cancers known as borderline operable in which there is scope for surgery but surgery would be difficult in view of tumour being adherent to major vascular structures
These patients are often considered for chemotherapy and sometimes radiation prior to surgery. Surgery for these cancers poses special challenges. Apart from Whipple’s operation the surgeon will have to be prepared for reconstruction of the main blood supply to the liver known as the portal vein and the hepatic artery
This surgery is potentially risky as blood supply to the liver and the small intestine is interfered with. These types of surgeries require good team of surgical oncologist, vascular surgery and anaesthetist and critical care
Let me describe such a complex surgery performed at Apollo Hospital, Bannerghatta Road
Patient was a 64-year-old gentleman who was diagnosed with a pancreatic cancer which had shown encasement of the major blood vessels to the liver namely the portal vein and hepatic artery. The PET scan however did not show and other area of metastases.
This was considered borderline operable and patient received chemotherapy first and then radiation. The treatment went on for almost 6 months
Following this a repeat scan showed stable disease. The disease had not spread anywhere else however the adherence to the blood vessels remained, it was at this time that we decided to go ahead with Whipple’s operation along with possible resection of the portal vein and hepatic artery
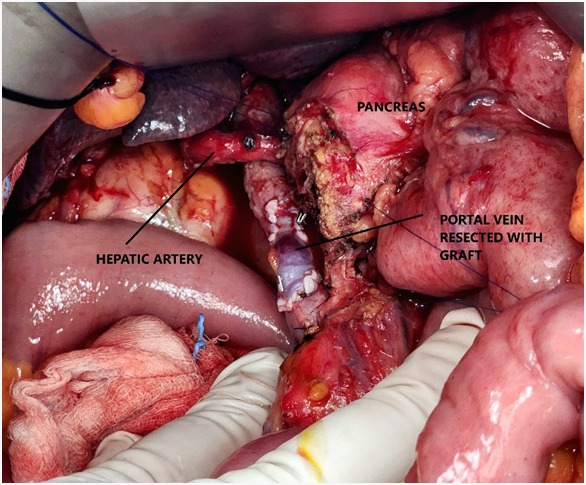
The surgery was challenging and the hepatic artery was carefully dissected out, the portal vein however could not be dissected and for this a part of the vein was resected along with the tumour. The defect in the portal vein was covered with a cadaver vein graft. The duration of surgery was 12 hours
Meticulous anaesthesia management was critical in this patient as clamping of the portal vein can lead to interference with the small bowel circulation leading to acid build up
The first two days in ICU were stormy with fluctuations in blood pressure and haemoglobin however the patient stabilized and was successfully shifted out of ICU and later discharged
This surgery though risky has offered the patient a good chance of cure and long-term survival